LYME DISEASE (Borreliosis)
A Plague of Ignorance Regarding the Ignorance of a Plague
© Copyright 2004, Dr Scott Taylor, DVM, All rights Reserved
My objective for writing this report is to help inform the layman and the medical community about the extremely complex infection called Lyme disease. I have recently been infected with Lyme disease and I will share my experience and what I have learned about the complex nature of Lyme disease in this report. I continue to update this report and I foresee many revisions of it in the future as more information regarding Lyme disease surfaces. I have recently been introduced to a major medical breakthrough discovered by Dr. Trevor Marshall, research director at the Autoimmunity Research Foundation in Thousand Oaks, CA. I have updated this version of the report to include this vital information.
Lyme disease (LD) is a seriously complex
multi-system inflammatory disease that is triggered by the bacterial
lipoproteins (BLPs) produced by the spiral-shaped bacteria called
Borrelia. Borrelia are difficult to isolate, grow, and study in the
laboratory. So, our technical knowledge of this pathogen is poor
compared to our understanding of most bacteria that cause disease.
Transmission of Borrelia occurs primarily through the bite of ticks.
The disease affects every tissue and every major organ system in the
body. Clinically, it can appear as a chronic arthalgia (joint pain),
fibromyalgia (fibrous connective tissue and muscle pain), chronic
fatigue, immune dysfunction and as neurological disease. LD may even be
fatal in severe cases.
The diagnosis of Lyme disease is primary based upon clinical evidence.
There is currently no laboratory test that is definitive for Lyme
disease. Many tests give false negative results. Physicians not
familiar with the complex clinical presentation of Lyme disease
frequently misdiagnose it as other disorders such as: Fibromyalgia or
Chronic Fatigue Immune Dysfunction Syndrome (CFIDS), Multiple Sclerosis,
Lupus, Parkinson's, Alzheimer's, Rheumatoid Arthritis, Motor Neuron
Disease (ALS, Amyotrophic Lateral Sclerosis -Lou Gherig's disease),
Multiple Chemical Sensitivity Syndrome (MCS) and numerous other
psychiatric disorders such as depression and anxiety.
Lyme disease is a familiar name to most people, but their knowledge of it is very limited. Unfortunately, this is also true for most professionals in the medical community. There have been numerous reports in the media about it in the United States over the past 25 years. These superficial articles report something about small deer ticks transmitting bacteria called Borrelia burgdorferi. The tick vectors are said to be mainly restricted to certain endemic areas of the United States, which are the Northeast and the upper Midwest. Frequently mentioned is the bulls-eye skin rash that develops following the bite of an infected tick. The disease is reported to begin with flu-like symptoms that progress to an arthritic and fibromyalgic condition. It is often said that Lyme disease can be readily treated with standard regimens of antibiotics. While these reports are partially true, they are also critically erroneous and very misleading!
This report is an urgent warning for everyone. Lyme disease is devastating the lives of hundreds of thousands of individuals and we are all at risk. Many patients are suffering with chronic Lyme disease and continue to be misdiagnosed and mistreated. In many cases of Lyme disease, a correct diagnosis doesn’t occur until after several months or more often many years of suffering with the disease. By then it has caused severe illness, disability and permanent damage. The disease is widespread and the prevalence is significantly higher than reported by health officials.
It is very unfortunate that most physicians don’t know how to recognize and treat cases of Lyme disease, especially the illusive cases of chronic Lyme disease. I’m not just talking about general MDs being ignorant; I am also referring to specialists such as: rheumatologists, neurologists, orthopedic surgeons, cardiologists, psychiatrists, and the most ignorant actually seem to be infectious disease specialists. I was extremely surprised by this plague of ignorance after I began my investigation of Lyme disease.
There are some key factors that exist in the medical community regarding Lyme disease; they go a long way in explaining why LD is often misdiagnosed and mistreated:
In the mid-1990's genospecies were formed to group the many variations into subcategories.
Borrelia burgdorferi sensu lato is name given to the overall category. In North America there is just one genospecies variant - Bb sensu stricto. In Europe there are three categories Bb sensu stricto, B. garinii, and B. afzelii. Asia has B. garinii and B. afzelii. Japan has B. japonica and B. miyamoto. These groups are evolving as new research discoveries occur.
A new pathogen causing Lyme or "Lyme-like" disease has been reported. While not culturable, it has been named B. lonestari sp.
B. andersonii, B. lonestari and B. miyamotoi have been identified by PCR and DNA sequence analysis as likely human pathogens in the U.S. Unfortunately, the criteria for clinical Lyme are set for only Borrelia burgdorferi; they were not designed for any other borrelia species. The reason that Borrelia burgdorferi is tracked by health officials but not other species is because it’s the primary borrelia species that laboratories are able to identify and study. I admit that Borrelia species are very difficult to grow (fastidious) and work with in the laboratory. In most cases, laboratories are not even able to isolate and identify Borrelia species. Some other known strains of borrelia include: B. valaisiana,
B. lusitaniae and B. bissettii.
Lyme Wise Medical Doctors: The Few, the Knowledgeable, the Harassed
The plague of ignorance surrounding Lyme disease makes it very controversial within the medical community. Most MDs are ignorant about the complex nature of Lyme disease and are frequently irritated when confronted about it. There are only a few MDs in the country that are knowledgeable about Lyme disease; they are often called Lyme literate MDs (LLMDs) by the Lyme aware public and by their Lyme patients. Most LLMDs know about Lyme disease because they have studied it independently. The MD’s formal training in medical school and from the established medical community regarding Lyme disease is meager.
LLMDs have been and continue to be harassed by the medical community, by health officials, by their peers and colleagues, by state medical boards, and by insurance companies for diagnosing and treating Lyme patients beyond the standards set by the establishment. Unfortunately, some of these LLMDs have discontinued treating Lyme patients due to the harassment. A few LLMDs have actually had their medical license revoked because they have treated Lyme patients beyond standards set by the medical community. For example, treating patients with antibiotics for longer than the standard 4-6 week period of time can lead to harassment.
If Lyme patients are lucky enough to find an LLMD and get the proper diagnosis and therapy, guess what? Many health insurance companies are declining to pay for the appropriate antibiotic treatment. Why? If it’s not the standard therapy established by the ignorant medical community, the insurance companies won’t pay. The Standard therapy for Lyme disease, which is considered to be a 4-6 week course of antibiotics, is too short for most Lyme cases. A basic treatment for chronic Lyme disease usually requires at least an 8 -16-month period of appropriate antibiotics.
Throughout my studies of conventional and alternative medicine, I often encounter the shortcomings of conventional medicine. Their ignorance surrounding Lyme disease (LD) may be one of conventional medicines biggest failures. In fact, I’d place it up there with their disastrous low-fat, low-calorie diet recommendation. I am extremely disappointed by what little they know and what little they do regarding Lyme disease. This ignorance should not exist. I have been able to educate myself about Lyme disease. There are plenty of good resources on the internet that are full of helpful information regarding Lyme disease. I have placed some links about LD on my site that can be found at: www.myremedi.com. The medical establishment needs to connect the complex clinical picture of Lyme disease with the evidence already present in the scientific literature. I know they won’t consider anecdotal evidence which is very helpful in understanding Lyme disease clinically, but isn’t considered scientific. Unfortunately, there isn’t enough clinical art mixed into conventional medicine.
The History of Lyme Disease
Lyme disease has a relatively young history in the U.S. The first reported case of borreliosis in the U.S. was made by Dr. Rudolph Scrimenti in 1970. He noticed a skin lesion called erythema migrans (EM), a rash that Borrelia can cause soon after a tick bite. Scrimenti diagnosed and treated the patient who had been bitten by a tick and acquired LD while hunting in Wisconsin. Lyme disease was later rediscovered in the well-known Lyme, Connecticut outbreak that began in 1975 by Dr. Allen Steere. He misdiagnosed this outbreak as juvenile rheumatoid arthritis near the community of Lyme, Connecticut. At that time the condition was named 'Lyme arthritis.’ Then, in the early 1980s, B. burgdorferi was recognized as the causative agent of the Lyme outbreak and the name was later changed to Lyme disease.
Although the disease was named for the town in Connecticut, Lyme disease (borreliosis) actually has a long history taking it as far back as the 1800s. The first reported case of clinical Lyme disease was made in Germany by Dr. Alfred Buchwald in 1883. He described a degenerative skin disorder now called acrodermatitis chronica atrophicans (ACA) that is known to be caused by Borrelia. Thus, a great deal of information was already known about Lyme disease prior to its rediscovery as Lyme disease in the United States. However, most of this early medical history of LD comes from the European scientific literature. The U.S. still lags behind the Europeans regarding their understanding of borreliosis.
The terminology used to describe Borrelia infections and the disease caused by them is not clearly defined. The name "Lyme disease" has been used to describe the illness specifically caused by only B. burgdorferi, not other Borrelia species. However, the term Lyme disease or Lyme borreliosis is commonly used to describe the infectious diseases that are caused by many Borrelia species. More appropriately the name for the disease caused by borrelia infections is borreliosis. However, borreliosis isn’t commonly used and is not familiar to most, so I will often use the more familiar name, Lyme disease. However, please note that I will use borreliosis, Lyme disease, or Lyme borreliosis interchangeably to describe the complex disease caused by borrelia infections.
The Spirochete Called Borrelia: What Makes Lyme Disease Tick
Borrelia species, like the human pathogen Treponema pallidum, (the cause of syphilis) are placed in the spirochete family of bacteria. Spirochetes are long, thin, spiral-shaped bacteria that have flagella (tails), (see figures 1 & 2 below). Other familiar humans diseases caused by Borrelia species include: 1) relapsing fever, which use soft ticks or lice as vectors, and 2) gum disease. The genus Brachyspira is a spirochete that commonly causes colitis in swine in Europe and has recently been discovered to cause colitis in humans.
Spirochetes are very difficult to grow (fastidious), identify, and study in the laboratory. In the laboratory we still cannot grow the spirochete that causes syphilis, Treponema pallidum. This makes it very difficult to perform research and develop better diagnostic tests and therapies for borreliosis. Borrelia species grow extremely slowly; they even grow slower than many fungi and mycobacteria. Their growth rate is also slower than Mycobacterium tuberculosis, which causes tuberculosis. Borrelia’s slow growth partially explains its ability to cause chronic disease and the difficulty identifying it in the laboratory.
Borrelia exists in three different life forms: 1) the cyst, 2) the spheroplast or "L form", which doesn’t have a cell wall (commonly called: cell wall deficient (CWD)), and 3) the typical spiral-shaped bacteria form that has a cell wall and flagella as seen in figures 1 & 2. Spirochetes have a unique mode of motility that allows them to easily travel through tissues of the body. By rotating their axial filament (endoflagella) the flagellum rotates causing the spirochete to actually move in a cork-screw fashion. This mode of motility allows spirochetes to literally "screw" themselves into and through the tissues of the body. They can also contract like a spring and move through tissue as they uncoil. Spirochetes hide their flagella from the host’s immune defenses, which are normally antigenic and would trigger an immune response if detected.
Figure 1
In 1982 the brilliant entomologist, Willy Burgdorfer, discovered the etiologic agent of Lyme disease. He was investigating ticks at the United States Rocky Mountain Laboratories located in Montana, part of the National Institutes of Health, when he isolated spirochetes from the mid-guts of Ixodes ticks. He showed that these spirochetes reacted with immune serum from patients that had been diagnosed with Lyme disease.
Consequently, the etiologic agent was named in his honor, Borrelia burgdorferi (Bb). It is interesting to note that Dr. Burgdorfer was familiar with European literature regarding borreliosis and was able to connect that information to the Lyme outbreak. I wish the rest of our medical establishment would be as diligent as he.


Figure 2: Borrelia burgdorferi, the bacteria that causes Lyme disease, left picture seen at 400x magnification. Right picture is a scanning electron micrograph of Treponema pallidum, the cause of syphilis.
Justified Arachnophobia: Ticks, the Vector of Borrelia
Ticks are bloodsucking external parasites that feed on humans, wild and domestic mammals, and birds. Ticks are not insects; they are 8-legged arachnids along with chiggers, spiders, and mites. The outbreak of Lyme disease in Lyme Connecticut back in 1975 occurred in a rural location and the onset of illness during the summer and early fall indicated that an arthropod vector was probably responsible for the transmission of the disease. As mentioned earlier, the primary method of transmitting LD was discovered to be through ticks.
I want to re-emphasize that there is a tremendous misunderstanding regarding the vector (carrier) that transmits Lyme disease. Again, the familiar tick vectors called the deer tick (Ixodes dammini) and black-legged tick (also commonly called deer ticks) (Ixodes scapularis) are more prevalent and spread wider than reported. These ticks are not the only vector able to transmit Borrelia species. Several other tick species including the Lone Star ticks (Ammblyoma americanum), western black-legged ticks (Ixodes pacificus), wood ticks or American dog ticks (Dermacentor variabilis) and the Brown dog tick (dogs are the only host for these ticks) can transmit it, too. Unfortunately, health officials are not reporting this critical information and thus, the public and medical community are not informed about this.
Since the widespread distribution of these tick vectors greatly increases the prevalence of Lyme disease well beyond that of official reports. The public needs to understand the potential danger of all tick bites, not only that from the deer tick.
 Figure 3
Figure 3
The Life Cycle of TicksTicks have a life cycle of 2 years that includes the egg, larvae, nymph, and adult stages, (see figure 3). Nymphs and adults appear to be primarily responsible for transmission of the borrelia to susceptible large animal hosts including humans; however, larvae can transmit borrelia to humans also.
In the spring, eggs hatch into a larvae ("seed" tick) that have six legs. Larvae feed and molt into nymph that have eight legs and no sex differentiation. Nymph feed and molt into adults that are differentiated into male or female. Similar to the mosquito, the adult female tick requires a blood meal before she can lay eggs.
A tick seeks a blood meal at or slightly above ground level by climbing onto vegetation and using its forelegs to feel and grab a host. They are usually found between ground level to three feet above the ground. To locate a host, a tick detects carbon dioxide, scent, body heat, and possibly other stimuli generated from the host’s body. Ticks generally feed once during the spring, but they may feed in the fall and anytime during the year. They are active at temperatures above 42° F. Although the incidence of Borrelia induced erythra migrans (EM) skin rashes is highest during the spring and early summer, symptoms of LD may occur anytime during the year.
Ticks cannot survive long exposure to the sun and are therefore typically found in shaded areas. Tick habitats must contain both small animal hosts for tick larvae and large animal hosts for tick adults. A relative humidity of greater than 65% is required for hatching eggs and larvae survival. This cool, wet spring of 2003 has been ideal for producing ticks. This means that there will be a large crop of feeding nymphs this fall and next spring; followed by a large crop of feeding adults throughout the year 2004.
A favorite tick habitat is the transitional zone between woods and lawns or meadows. Ticks become stimulated by the warmth and carbon dioxide that is produced by a host that spends a considerable amount of time in the ticks’ environment. Ticks will grab a passing host or drop to the ground, find the host, and climb onto it. They will travel upward until they reach the head or are obstructed. It is important to remember that humans can be hosts for all stages of ticks.
The deer tick is the size of a pinhead in the larvae stage. It is tan, and feeds on small animals like the mouse where it can pick up the spirochete. During the nymph stage the tick is the size of a poppy seed. It is beige or partially transparent and feeds on larger animals such as cats, dogs and humans. Adult deer ticks are black and/or reddish and will feed on cattle, deer, dogs and humans.
Figure 4: Left is the Amblyomma americana (Lone Star tick) nymph, adult, and larva. Center is the Dermacentor variabilis (American dog or wood tick) adult. Right is the Ixodes scapularis (black-legged tick) larva, adult, and nymph.

Figure 5: Lone Star tick, Amblyomma americanum
The Loan Star ticks get their common name from the single silvery spot located on the female's back (see figure 5). Lone star ticks attack humans more frequently than any other tick in the eastern and southeastern states. Its distribution occurs from west-central Texas northward to Iowa and eastward to the Atlantic Coast. It is especially abundant in the Ozark region and eastern Oklahoma. Recent evidence indicates that the Lone Star tick may play a major role as a vector for Borrelia species, e.g., Borrelia lonestari, in the South and Midwest. Unfortunately health officials are not alerting the public about this significant threat. The most common of all ticks in the Midwest is the wood tick or dog tick.
 Figure 6:
Figure 6:
Comparison of the Capitulum (head/mouth) of the lone star tick (Amblyomma americanum) which clearly has a different size and shape than that of the American dog tick (Dermacentor variabilis).
Below-Magnified mouthparts of the deer tick (I. dammini)
Figure 7
Figure 7 is a CDC chart showing the distribution of the deer (Ixodes scapularis) and western black-legged (Ixodes pacificus) ticks. Unfortunately, this chart doesn’t show the large distribution of the Lone Star tick, American Dog Tick, Black-Legged Tick and other tick vectors of Borrelia. Again, according to the deficient reporting by the CDC there are three main focal points in the eastern half of the country, (see figure 8).
Ticks are carried by a number of different host animals, not simply deer. The hosts for adult ticks are numerous and include: fox, coyote, dogs, cats, cattle, rabbit, skunk, raccoon, rats, squirrels, white-tailed deer, wild turkey, and humans. Nymphs get on many of these same animals as well as larger animals typical for adults. Ground nesting birds including bobwhite quail, pheasants, turkeys and chickens are also tick hosts. Forty-nine species of migrating birds have been found to carry ticks, transporting them large distances and contributing to the national spread of Lyme disease. Potential minor vectors for Borrelia species include: chiggers, mosquitoes, biting flies and fleas. Cases of LD being contracted from infected pets are well documented; likely due to the pet bringing infected ticks into the home. Borrelia can also be transmitted in utero from an infected mother to a child during pregnancy. Congenital transmission can cause miscarriages, severe neurological disabilities, or other major system dysfunctions to the baby. Other modes of transmission probably exist that we are not aware of. I am personally concerned that transmission may occur through blood transfusions without authorities knowing about it.
Lyme Disease in the U.S.A.
Even epidemiological reports based on CDCs criteria, which significantly underestimate the true clinical prevalence by 10-15 times, show that Lyme disease has increased dramatically to the point that the disease has become an important public health problem in the United States. Lyme disease is the most prevalent tick-borne illness in the U.S. LD cases have been reported in all of the continental United States and on several different continents.
 Figure 8
Figure 8
By looking at this map, it is interesting to highlight certain points:
Figure 9
In 1996, there were 16,455 new cases reported in the U.S. The number dropped in 1997(see table above), but in 1998 there were 16,801 cases, and in 1999 there were 16,273 new cases reported to the CDC. In 2002, 18,000 cases of Lyme disease were reported in the U.S.
Reported cases of Lyme disease in 2002 were up nearly 40 percent from 2001,
according to the CDC. The phenomena does not appear to be regional, as 95 percent of
reporting states showed an increase in reported cases, with a one year
doubling seen in some states. The northeastern and northcentral states
remain a focus of concern, accounting for
approximately 90 percent of all cases.
With 23,000 new cases of Lyme reported last year, it is becoming
apparent that the disease is a much larger problem than many had
originally thought. CDC statements acknowledge the prevalence of Lyme
disease.
The Iowa Department of Public Health criteria for Lyme disease is actually much more restrictive than the CDCs criteria. A Lyme disease case must have three out of these five criteria:
Since 1982, 220 cases that fit the above criteria have been reported to the Iowa Department of Public Health. Twenty-six cases were reported in 1998. Wisconsin (5,970 cases since 1982), Minnesota (2,385 cases since 1982), and Missouri (1,060 cases since 1982) are all CDC endemic areas for Lyme disease.
Although Lyme is a mandatory reportable disease, physicians will often treat patients with early Lyme without getting positive serology tests and avoid reporting it to the Dept. of Public Health.
Pathogenesis of borreliosis: How Borrelia Cause
a Self-Perpetuating Inflammatory Disease
Understanding how borrelia causes disease is the key to successful diagnosis and treatment.
Bacterial Lipoproteins (BLPs)
Regarding borreliosis, the molecular component of the pathogen that appears initiate the pathogensis are the bacterial lipoproteins (BLPs) which are found within the outer surface proteins of the borrelia cell membrane.
BLPs are fat-soluble toxins that are part protein and part lipid. They are often a structural part of the borrelia cell membrane and can be found within the outer surface proteins of borrelia. They are very potent immunomodulators even in small amounts. Thus, a few borrelia can produce enough BLPs to initiate significant disease.
These BLPs trigger many harmful responses in any tissues and organ system of the human body. These responses, produce complex symptoms of fibromyalgia, arthritis, neurological signs, psychiatric disorders, immunologic dysfunctions, and endocrine deficiencies.
At the molecular level, the BLPs cause a dysfunction in the immune system by triggering a complex imbalance of chemical immune mediators (cytokines). These cytokines regulate the immune system and when they are over stimulated, they produce harmful reactions from the immune system, such as pain, inflammation, and even apoptosis (cell death). Some of the cytokines involved include: tumor necrosis factor-alpha (TNF-α), interleukins-6 (IL-6), fatty acid products (eicosanoids such as inflammatory prostaglandins, thromboxanes, and leukotrienes) that have potent inflammatory/physiological properties and many other cytokines play a role in the pathogenesis of borreliosis.
These BLPs have a key component, Pam3cys, which triggers an innate immune response that cascades into the disease borreliosis.
The inflammation triggered by the fat-soluble BLPs toxins is responsible for most, if not all symptoms of borreliosis.
So, the innate immune system and the acquired immune system are strongly triggered by the presence of the borrelia BLPs.
Toll-like Receptors and Innate Immunity
BLPs activates the innate immune system through what are called Toll-like receptors. Many cell types throughout the body carry the TLR receptors. It's a basic innate immune response that even invertebrates have. These receptors are able to recognize molecular patterns that are unique to microbial pathogens. The body uses TLRs to detect the prescence of many microbial pathogens, not just borrelia. The figure below shows how TLRs can detect several molecular patterns of different microbial pathogens. The TLRs that are most likely involved in borreliosis are TLR 2, 6, & 1, but TLR-2 likely plays the major role.
For a thorough review of the TLR signaling pathway see this reference: Seminars in Immunology 16 (2004) 3–9 ,TLR signaling pathways, by Kiyoshi Takeda, Shizuo Akira. Here’s the abstract from this manuscript:
Abstract
Toll-like receptors (TLRs) have been established to play an essential role in the activation of innate immunity by recognizing specific patterns of microbial components. TLR signaling pathways arise from intracytoplasmic TIR domains, which are conserved among all TLRs. Recent accumulating evidence has demonstrated that TIR domain-containing adaptors, such as MyD88,
TIRAP, and TRIF, modulate TLR signaling pathways. MyD88 is essential for the induction of inflammatory cytokines triggered by all TLRs. TIRAP is specifically involved in the MyD88-dependent pathway via TLR2 and TLR4, whereas TRIF is implicated in the TLR3- and TLR4-mediated MyD88-independent pathway. Thus, TIR domain-containing adaptors provide specificity of TLR signaling.
We know that BLPs are potent activators of Toll-like receptor-2 (TLR2). Thus, through TLR2, BLPs induces the synthesis of the precursor of the pro-inflammatory cytokine interleukin -1B (IL-1B). As shown in the figure below, TLRs can activate a transcription factor known as NF-kappa B which stimulates the gene expression for inflammatory cytokines.
BLPs also activates caspase 1 and potentiates apoptosis (programmed cell death) via this route.
The lipid moiety of the BLPs contains a part that is responsible for triggering the TLRs. A synthetic analog of this moiety is called: tripalmitoyl-S-glyceryl-Cys-Ser-Lys4-OH (Pam3Cys).
Other important inflammatory mediators triggered by BLPs in immune cells are tumor necrosis factor-alpha (TNF-α), IL-6, IL-12, INF-γ, and nitric oxide (NO).
A Major Medical Breakthrough; Dr. Trevor Marshall’s Angiotensin Discovery
The following discovery by Dr. Marshall shows how a Th1 inflammatory response can become self-perpetuating via the following biochemical pathway. Please note that sarcoidosis has a very similar pathogenesis to borreliosis. Borreliosis may actually cause many cases of sarcoidosis.
The Angiotensin Hypothesis
New Treatments Emerge as Sarcoidosis Yields Up its Secrets
Authors:
Trevor G. Marshall, Ph.D.,
SarcInfo, Thousand Oaks, California, trevor.m@yarcrip.com
Frances E.(Liz) Marshall, Grad. Dipl. Pharm,
Los Robles Regional Medical Center, Thousand Oaks, California, liz.m@yarcrip.com
We have concluded that sunlight fuels the inflammation of sarcoidosis, via 1,25-D and Angiotensin II, in the following manner:
As the circulating concentration of 1,25-D increases within the inflamed tissue, a much larger quantity of hematopoetic stem cells differentiate to produce monocytes . Monocyte differentiation into macrophages and epithelioid giant cells is enhanced. The differentiating macrophages and giant cells release Angiotensin Converting Enzyme. This ACE catalyzes Angiotensin I to form Angiotensin II (A-II). The A-II then binds at A-II Type 1 receptors on the macrophages and activated T-lymphocytes , stimulating Nuclear Factor-kappaB (NF-κB) to signal the release for a cascade of Th1 cytokines . At least one of these cytokines, Gamma Interferon, increases the amount of 25-D being converted to 1,25-D in the macrophages, which in turn catalyses the differentiation of monocytes into even more macrophages and giant cells.
Normally this inflammatory cycle is self-limiting, but, in the case of sarcoid patients, 1,25-D levels are poorly controlled, leading to upregulated production of monocytes, and their upregulated differentiation into the macrophages and epithelioid giant cells characteristic of sarcoid granuloma.
Reichel, et al, demonstrated that lipopolysaccharide from gram-negative bacteria stimulated the generation of 1,25-D within pulmonary alveolar macrophages from sarcoid patients. A bacterial pathogenesis is therefore consistent with the initial increase in paracrine 1,25-D concentrations needed to trigger the run-away inflammatory biochemistry described above.
The blockade of A-II Type 1 receptors has been shown (in-vitro) to reduce production of the Th1 cytokines, including TNF-α, an action which would interdict this inflammatory process.
Angiotensin Receptor Blockers are currently indicated for hypertension. There is thus a simple clinical test of this hypothesis available for patients who are suffering both from Sarcoidosis and mild hypertension.
We have found that Benicar (Olmesartan Medoxomil), administered as 40mg every 6 to 8 hours, provides a very effective angiotensin blockade.
There are two issues
in the selection and dosage of the ARB. As you can see from the pressor
effect vs. dosage for Benicar (Figure 1), about 90% of the ultimate
pressor effect can be achieved with only 40mg, once per day. But this
dose is not well tolerated by sarcoid patients. Partly this may be the
result of the additional Angiotensin receptors in the inflamed tissues,
all of which have to be blocked, and partly it may be due to an
increased production of serum ACE by macrophages in  response
to the partial blockade. Sarcoid patients experience symptoms ranging
from increased fatigue to psychedelic dreams when prescribed ARBs just
once daily, the customary prescription for hypertension
response
to the partial blockade. Sarcoid patients experience symptoms ranging
from increased fatigue to psychedelic dreams when prescribed ARBs just
once daily, the customary prescription for hypertension
To be fully effective, we found that Benicar must be prescribed to sarcoidosis patients as 40mg every 6 to 8 hours. We found the ARB Diovan (Valsartan) to be less effective than Benicar, but it may be used at the 80mg q8h described in our earlier paper. Two patients reported sinus congestion with the Diovan blockade, which was not present after changing to Benicar. Controlled studies are needed to accurately define the blockade capability of each ARB, individually and in combination.
In summary, Dr. Marshall’s discovery reveals that during the pathogenesis of borreliosis the BLPs of borrelia trigger inflammation via TLR signaling pathways or by other intracellular activation of NF-kappa B, which stimulates the gene expression for inflammatory cytokines. When the inflammatory cascade goes chronic, it eventually goes into the self-perpetuating cycle described by Marshall. This cycle will continue to produce disease until it is stopped by intervention.
In my opinion, Dr Marshall’s discovery that A-II perpetuates a TH1 inflammatory cascade is nothing short of major medical breakthrough.
Dr. Marshall’s work has not only given us the model for the pathogenesis, he has also given us the therapeutic approach that breaks the perpetual cycle that maintains the inflammatory cascade.
Angiotensin II type 1 receptor blockade. The angiotensin receptor blocker (ARB) called Benicar (olmesartan medoxomil) has specific ARB properties that block this self-perpetuating inflammatory cascade.
Benicar therapy is a medical miracle for those suffering with chronic borreliosis.
Inducible Nitric Oxide synthase (iNOS) and its role in pathogenesis
TLR activation of the a transcription factor known as NF-kappa B stimulates the gene expression of inducible nitric oxide synthase (iNOS). In this way, BLPs can trigger an increased production of nitric oxide as the following reference note:
Vet Immunol Immunopathol. 1999 Feb 22;67(3):271-84.
Up-regulation of inducible nitric oxide synthase mRNA in dogs experimentally infected with Borrelia burgdorferi.
Harter L, Straubinger RK, Summers BA, Erb HN, Appel MJ.
James A. Baker Institute for Animal Health, College of Veterinary Medicine, Cornell University, Ithaca, NY 14853, USA.
Comparing the number of borrelia-positive tissues in dogs within Group A (acute
lameness) it was interesting to note that the dogs investigated on the first day of lameness
showed more borrelia-positive tissues than dogs from Days 2±4 of lameness. The mean of
the seven dogs with 1-day lameness was 72%, whereas the mean of the 3-day lameness
dogs was 36% (the single value for the 2-day lameness is 48%, for the 4-day lameness is
36%). This apparent decrease of the borrelia load during an episode of acute Lyme
arthritis may be a result of the host's inflammatory response. In contrast, the number of
iNOS-positive tissues increased from 40% for dogs with 1-day lameness to 64.3% for the
dog A96-2/3 with the 4-day lameness. While this might suggest the role for NO in
clearing B. burgdorferi from the infected tissues, the number of dogs investigated was not
sufficient to establish a reliable relationship between the borrelia load and the number of
iNOS-positive tissues during lameness. Further studies should clarify this point. The
milder and generally subclinical chronic Lyme arthritis, as represented by dogs from
Group B, is characterized by a lower number of borrelia-positive tissues and a lower
number of iNOS-positive tissues as well.
Immunol Lett. 1994 May;40(2):139-46.
Killing of Borrelia burgdorferi by macrophages is
dependent on oxygen radicals and nitric oxide and can be enhanced by
antibodies to outer surface proteins of the spirochete.
Modolell M, Schaible UE, Rittig M, Simon MM.
Max-Planck-Institut fur Immunbiologie, Freiburg, Germany.
Interaction of B. burgdorferi organisms with mouse bone marrow-derived
macrophages (BMM phi) leads to phagocytosis of microorganisms, induction
of nitric oxide (NO) and superoxide radicals (O2-) by BMM phi and
killing of spirochetes. Destruction of spirochetes by BMM phi was
quantified by a new method based on the release of radioactivity from
spirochetes pre-labelled with [3H]adenine. Uptake of B. burgdorferi by
BMM phi, which mainly occurs by coiling phagocytosis, generation of NO
and O2- radicals as well as killing of spirochetes were significantly
enhanced by pre-opsonization of spirochetes with monoclonal antibodies
(mAb) to the outer surface proteins A and B but not with those to the
periplasmic flagellin. Addition of inhibitors specific for NO and O2-
radical synthesis either separately or together to cultures of BMM phi
and spirochetes resulted in only partial reduction of the killing
potential of effector cells. The data indicate that NO and O2- radicals
are necessary, but not sufficient, for complete elimination of B.
burgdorferi by macrophages. Together with previous findings that
protection against B. burgdorferi infection is conveyed by humoral
immune responses the present data indicate that one of the important
functions of specific antibodies is their participation in
macrophage-mediated control of spirochetes.
Decreased nitric oxide-mediated natural killer cell activation in chronic fatigue syndrome.
Ogawa M, Nishiura T, Yoshimura M, Horikawa Y, Yoshida H, Okajima Y,
Matsumura I, Ishikawa J, Nakao H, Tomiyama Y, Kanayama Y, Kanakura Y,
Matsuzawa Y.
Osaka University Medical School, Osaka, Japan.
BACKGROUND: L-Arginine (L-Arg), one of the essential amino acids, has
been reported to have an immunomodulatory effect. The precise mechanism
of the L-Arg-induced natural killer (NK) cell activation remains
unresolved,and the effect of L-Arg on NK cells in chronic fatigue
syndrome (CFS) patients has not been estimated. METHODS: NK cell
function was evaluated in 20 subjects with CFS and compared with that in
21 healthy individuals. RESULTS: In healthy control subjects, NK
activity was significantly increased after treatment with L-Arg, an NK
function enhancer, for 24 h, whereas the same treatment failed to
enhance NK activity in the CFS patients. We thus focused on L-Arg
metabolism, which involves nitric oxide (NO) production through NO
synthase (NOS). The expression of inducible NO synthase (iNOS)
transcripts in peripheral blood mononuclear cells was not significantly
different between healthy control subjects and CFS patients. The
L-Arg-mediated NK cell activation was abolished by addition of
NG-monomethyl-L-arginine, an inhibitor for iNOS. Furthermore, incubation
with S-nitroso-N-acetyl-penicillamine, an NO donor, stimulated NK
activity in healthy control subjects but not in CFS patients.
CONCLUSION: These results demonstrate that the L-Arg-induced activation
of NK activity is mediated by NO and that a possible dysfunction exists
in the NO-mediated NK cell activation in CFS patients.
Infect Immun. 1994 Sep;62(9):3663-71.
Outer surface lipoproteins of Borrelia burgdorferi stimulate nitric oxide production by the cytokine-inducible pathway.
Ma Y, Seiler KP, Tai KF, Yang L, Woods M, Weis JJ.
Department of Pathology, University of Utah School of Medicine, Salt Lake City 84132.
The outer surface lipoproteins of Borrelia burgdorferi, OspA and OspB, stimulate the production of nitric oxide (NO) by murine bone marrow-derived macrophages from BALB/c, C3H/HeN, and C3H/HeJ mice. Gamma interferon (IFN-gamma) caused a three- to fivefold enhancement of this production of NO, and the L-arginine analog N-guanidino-monomethyl L-arginine inhibited it. Activation of transcription of the inducible NO synthase gene in stimulated macrophages was demonstrated by reverse transcriptase rapid PCR. Although IFN-gamma increased the amount of NO produced in macrophage cultures, it did not cause transcription of the inducible NO synthase gene greater than that seen with the Borrelia proteins. OspA and OspB also induced the production of high levels (40 to 150 ng/ml) of IFN-gamma in cultures of macrophages incubated with interleukin-2 (IL-2)-elicited cells from normal (T and NK cells) and scid (NK cells) mice but not in macrophages or IL-2-elicited cells cultured individually. This suggests that OspA stimulated macrophage production of cytokines, which, in turn, stimulated the production of IFN-gamma by NK and T cells. Reverse transcriptase rapid PCR demonstrated that OspA and sonicated B. burgdorferi stimulated production of several inflammatory cytokines in macrophage cultures, including IL-1, IL-6, IL-12, IFN-beta, and tumor necrosis factor alpha. As tumor necrosis factor alpha, IFN-beta, and IL-12 are potent activators of IFN-gamma production by T and NK cells, their presence in these cocultures could be responsible for the IFN-gamma production. Lymphocytes from infected C3H mice also produced IFN-gamma when stimulated with B. burgdorferi; thus, immune cells may also modulate NO responses. The generation of NO during infection with B. burgdorferi may be important, as NO has potent antimicrobial properties. NO can also be involved in pathological inflammatory processes in which its generation is detrimental to the host. Thus, the colocalization of B. burgdorferi lipoproteins, NO-producing cells, and regulatory cytokines may determine the outcome of infection.
Borrelia lack the microbial toxins called lipopolysaccharides (LPS) however, they have over 150 genes that encode for the BLPs that are the key to their pathogenicity. This is over 50 times greater than other pathogenic bacteria. That is, other bacteria usually only have 3 genes for lipoproteins, while borrelia have 150!
With this many BLPs triggering an imbalance of the immune system and other innate responses in the body, it’s not hard to see how a cascade of chronic problems can arise from this.
For example, when we look at psychological problems of neuroborreliosis, it’s clear that the cause of these symptoms arise from BLPs triggering encephalitis and that this inflammation not only causes imbalances in numerous neurotransmitters, it also causes vasculitis which leads to hypoperfusion and hypoxia of the brain.
These toxins also cause a channelopathy, which lead to a dysfunction of signals along neurons, muscles and cells making them easily excitable, but not able to discharge correctly…since the electrical potential across the cell membranes don't function normally.
This can attribute to numerous symptoms such as anxiety, paresthesias, hyperacusis, tremors and even susceptibility to static shock that many LD patients have.
Thus, the evidence is pretty clear that BLPs plays a large role in the pathogenesis of borreliosis and is a key to understanding this disease.
IMO, without BLPs, borrelia would not be virulent.
Some questions I’ve received regarding the pathogenesis of borreliosis:
Q: I don't see anything so far that would describe why these inflammatory mediators, which would be activating the T-cells, would not be phagocytized by these and other macrophages.
A: Initially it does. The initial infection of borrelia can be acute and flu-like or it may not even be noticable. Unfortunately, this initial immune response doesn't completely rid the body of borrelia.
I don't think we have the complete answer to why this happens. But there are probably several factors involved. Borrelia can adapt and be very stealthy. Another reasonable theory is that apoptosis of monocytes, macrophages, neutrophils and other immune cells triggered by TLR-2 stimulation may account for immune dysfunction and supression.
This makes a lot of sense to me since we see immune dysfunction & suppression in chronic LD and in CFIDS, which I believe have a very similar pathogenesis.
Q: Also, if it's somehow a more severe activation of these mediators,
especially if caspase and IL-12 are involved, why is there not more
obvious toxic shock-like symptoms apparent early on?
A: I wouldn't say that it's a more severe activation of these mediators, but more of a long term chronic/relapsing imbalance of them.
It may also have to do with borrelia's ability to grow slowly and not trigger an acute toxic shock.
It also may have something to do with borrelia's ability to hold on to it's BLPs and not release them into the surrounding tissue until they are killed.
We know that when we kill borrelia (such as with abx tx) the BLPs are released from them and we experience a herx reaction. In severe cases this response can be quite acute.
There are probably several other factors such as lipid depot effect and slow release.
The immune supressing effect of BLPs likely plays a role here too.
Q: It seems that many people are not even symptomatic until years after the original tick exposure.
A: This is true with borreliosis...(this happened in my case). It's also true with syphilis.
This may be due to borrelia's ability to code for so many different BLPs. They have the genetic code for over 150 different BLPs.
Depending on which ones and how strong the expression of these BLPs genes are may determine how virulent the borrelia is at different times.
We know that borrelia change the expression of these genes when exposed to different environmental factors such as temperature.
They express different BLPs in ticks since they are in ambient temperature, but once inside a mammal, they begin to change the BLPs that they express.
They also have an effective ability to accept plasmids and pick up other pathogenic genes in this way.
Work has shown that removing certain BLPs from virulent strains makes the borrelia avirulent.
The evidence is very suggestive that BLPs determines the pathogenesis of borrelia.
This work has appeared very timely for this discussion:
J Infect Dis. 2004 Jan 1; 189(1): 113-9. Epub 2003 Dec 22
Selective Induction of Matrix Metalloproteinases by Borrelia burgdorferi via Toll-Like Receptor 2 in Monocytes.
Gebbia JA, Coleman JL, Benach JL.
Center for Infectious Diseases, Centers for Molecular Medicine, and State of New York Department of Health, Stony Brook University, Stony Brook, New York, USA.
Regulation of secretion of matrix metalloproteinase (MMP) underlies the basis of numerous physiological and pathological processes in multicellular organisms.
The Toll receptor family, which is conserved from Drosophila species to humans, mediates pattern recognition of a diversity of ligands involved in morphogenesis and innate immunity. Here, we show that secretion of MMP-9 is selectively induced through Toll-like receptor (TLR) 2 in human and murine monocytic cells stimulated with Borrelia burgdorferi.
Secretion of MMP-1 was shown to be stimulated through a pathway other than TLR2, under identical conditions. Analysis of nuclear extracts indicated that activator protein (AP)-1 was reduced in TLR2-neutralized monocytic cells, suggesting that AP-1 plays a role in the transcriptional activation of MMP-9 through TLR2.
The specific induction of MMP-9 through TLR2 provides direct evidence of a new role for this ancient receptor family in regulating secretion of MMPs and demonstrates evolutionary convergence between invertebrate morphogenesis and the vertebrate innate immune system.
Gulf-War-Syndrome (GWS) has very similar symptoms to chronic borreliosis.
Mycoplasma fermentans is being considered to be the likely pathogen...whether it is or not, it's likely some BLP producing microbe is.
Since the symptoms are similar, I'd expect the pathogenesis would be similar.
Work such as this indicates that this may be the case:
Stimulation of human Toll-like receptor (TLR) 2 and TLR6 with membrane lipoproteins of Mycoplasma fermentans induces apoptotic cell death after NF-kappaB activation.
Into T, Kiura K, Yasuda M, Kataoka H, Inoue N, Hasebe A, Takeda K, Akira S, Shibata KI.
Departments of Oral Pathobiological Science and Oral Health Science, Hokkaido University Graduate School of Dental Medicine, Nishi 7, Kita 13, Kita-ku, Sapporo 060-8586, Japan. Department of Host Defense, Research Institute for Microbial Diseases, Osaka University, 3-1 Yamada-oka, Suita, Osaka 565-0871, Japan.
Mycoplasmal membrane diacylated lipoproteins not only initiate proinflammatory responses through Toll-like receptor (TLR) 2 and TLR6 via the activation of the transcriptional factor NF-kappaB, but also initiate apoptotic responses.
The aim of this study was to clarify the apoptotic machineries. Mycoplasma fermentans lipoproteins and a synthetic lipopeptide, MALP-2, showed cytocidal activity towards HEK293 cells transfected with a TLR2-encoding plasmid.
The activity was synergically augmented by co-expression of TLR6, but not by co-expression of other TLRs. Under the condition of co-expression of TLR2 and TLR6, the lipoproteins could induce maximum NF-kappaB activation and apoptotic cell death in the cells 6 h and 24 h after stimulation respectively.
Dominant-negative forms of MyD88 and FADD, but not IRAK-4, reduced the cytocidal activity of the lipoproteins. In addition, both dominant-negative forms also downregulated the activation of both NF-kappaB and caspase-8 in the cells.
Additionally, the cytocidal activity was sufficiently attenuated by a selective inhibitor of p38 MAPK.
These findings suggest that mycoplasmal lipoproteins can trigger TLR2- and TLR6-mediated sequential bifurcate responses: NF-kappaB activation as an early event, which is partially mediated by MyD88 and FADD; and apoptosis as a later event, which is regulated by p38 MAPK as well as by MyD88 and FADD.
In regards to this and other work showing that BLPs stimulates MMP-9, what this means is that the BLPs of borrelia have the ability to turn our own immunes system against the extracellular proteins of our body.
Extracellular proteins (ECP) make up the "mortar" between our cells, ie, it’s what holds the cells together in tissues.
There are several proteins in ECP: collagen, elastin, gelatin, and several others.
BLPs have the ability (thru TLR-2) to trigger our immune system to produce and release protease enzymes that digest these important ECPs. These include proteases such as collegenase, and elastase.
This protease activity is very damaging to tissues and itself can stimulate even more inflammation.
Borrelia takes advantage of these protease enzymes to penetrate through the tissues of the body. As ECPs are digested in tissues it is easier for borrelia to move through it.
This portion of the pathogenesis of borrelia explains a lot of the fibromyalgia symptoms in LD.
IMO, FMS/CFIDS and borreliosis/Lyme disease have a similar pathogenesis, which is TLR triggering by the BLPs or LPS of pathogenic microbes.
Borrelia also have an affinity for the endothelial cells lining the inside of blood vessels. They attach and infect the endothelial cells of blood vessels and trigger inflammation in these infected blood vessels (vasculitis) wherever they reside in the body. In other words, once the Borrelia infects the endothelial cells, they stimulate vasculitis of the blood vessel. Vasculitis of the nervous system, skin, muscle, tendons, and connective tissue explains much of the disease and clinical symptoms caused by Borrelia.
Borrelia species have several other characteristics that make them a challenging pathogen. They can reside and grow intracellularly (inside the cells); out of reach of the host’s immune system. By rotating their filaments, the spirochetes are able to move throughout the body in a corkscrew fashion; invading tissue, penetrating cells, replicating, and destroying the host cells they infect. The spirochetes hide their flagella, which are normally antigenic, from the host immune defenses. As Borrelia emerge from host cells they can wrap themselves with the membrane of the host cell, thus concealing themselves from the hosts immune system.
Borrelia’s ability to grow slowly and avoid attack by the host’s immune system makes it a difficult pathogen to destroy. Not only can borrelia evade the host immune system, but often will suppress it as well.
It’s also important to remember that borellia can go dormant in the body for lengthy periods of time. Then it can return to cause disease at any time.
The Early Symptoms of Lyme Disease
 It’s important to remember that fewer than 50%
of patients with LD will initially have the skin rash called erythema
migrans (EM). An EM rash with a round red ring and a central clearing
(see figure 10) is called a bulls-eye rash and it is diagnostic for Lyme
disease. In other words, a bulls-eye rash is enough evidence to
confirm a diagnosis of LD. However, I emphasize that EM is seen in less
than 50% of infected individuals with Lyme disease. The reason I
stress this is because many physicians think they must see an EM rash
and have laboratory confirmation before they will make a diagnosis of
Lyme disease. But, if less than 50% of LD cases have an EM rash,
physicians misdiagnose these early clinical cases of Lyme disease and
the prognosis for these mistreated patients deteriorates with time.
It’s important to remember that fewer than 50%
of patients with LD will initially have the skin rash called erythema
migrans (EM). An EM rash with a round red ring and a central clearing
(see figure 10) is called a bulls-eye rash and it is diagnostic for Lyme
disease. In other words, a bulls-eye rash is enough evidence to
confirm a diagnosis of LD. However, I emphasize that EM is seen in less
than 50% of infected individuals with Lyme disease. The reason I
stress this is because many physicians think they must see an EM rash
and have laboratory confirmation before they will make a diagnosis of
Lyme disease. But, if less than 50% of LD cases have an EM rash,
physicians misdiagnose these early clinical cases of Lyme disease and
the prognosis for these mistreated patients deteriorates with time.
Figure 10: The presentation of erythema migrans in early borreliosis
If present, the EM rash appears between 3 days to 1 month following the bite of an infected tick; however, the rash typically resolves itself spontaneously over a 2-4 week period. The EM rash grows concentrically over the following 5-10 days and without treatment may last for up to several weeks. The rash can vary from very small to very large (up to twelve inches across). Unfortunately, the EM rash is not the only rash associated with Lyme. Various other rashes associated with LD have been reported. One tick bite can cause multiple rashes. The rash can mimic such skin problems as hives, eczema, sunburn, poison ivy, fleabites, etc. The rash can itch, feel hot or it may even be asymptomatic and go unnoticed. The rash can disappear and return several weeks later. I recommend taking a photograph of any rash, especially if associated with a tick bite. The photos will help the Lyme knowledgeable physician make a proper diagnosis and prescribe the appropriate treatment.
All rashes that occur at the site of a tick bite are not due to Lyme disease. An allergic reaction to tick saliva often occurs at the site of a tick bite. This rash can be confused with the rash of Lyme disease. Allergic reactions to tick saliva usually occur within hours to a few days after the tick bite; they usually do not expand and disappear within a few days. EM rashes caused by Lyme disease persist longer, but usually subside within a few weeks.
The occurrence of multiple EM skin rashes is indicative of systemic spread of the organisms. Multiple EM lesions usually do not occur until after 2-4 weeks following the initial tick bite. This is the same time period during which the organisms are being spread throughout the body to other tissues and cells.
Borrelia Slowly Spreads Throughout the Body -- Approximately 4-6 weeks following the tick bite, the first systemic signs of Lyme disease that may or may not occur are in the form of flu-like symptoms or malaise. These symptoms include sore throat, severe headaches and neck aches, severe fatigue, chills and fever, and swollen lymph nodes. Upper respiratory symptoms are usually not present with LD, distinguishing it from other flu-like illnesses. While the LD-flu symptoms can spontaneously resolve themselves, patients can experience relapses.
Soon after the onset of Lyme-flu, arthralgias and/or myalgias (muscle and joint pain) may begin. The arthralgias appear to primarily involve the large joints (i.e. knees, elbows, hips, shoulders), although smaller joints (e.g. wrists, hands, fingers, toes) may be involved. The pains are generally described as severe, jumping from joint to joint, and may be present for only short periods of time. Pain in the teeth and in the temporal-mandibular joints (jaw) is common. Neurological involvement will cause associated paresthesias (muscle twitching, burning sensations, prickling / shooting pains, and numbness). Lyme disease can cause palsy of affected areas, but it’s more likely to cause neurosensory deficits before neuromotor disease.
Facial nerve (Bell's) palsy is another neurological symptom of Lyme disease. Encephalitis or encephalopathy may manifest as cognitive dysfunction, including short-term memory loss, and psychiatric symptoms such as panic, anxiety, or depression. The encephalitis and facial paralysis tend to occur within the first few months following the tick bite, but may also occur as part of a relapse at any time.
Other symptoms in this stage of the disease may include blurred vision, uveitis, ringing in the ear (tinnitus, which was one of my first symtoms) and/or hearing loss, shortness of breath, palpitations or tachycardia (rapid heart rate), chest pains, abdominal pains, diarrhea or irritable bowel, testicular or pelvic pain, urinary incontinence/urgency, dizziness, tremors, dysautonomia, and hepatitis.
Borreliosis: The Clinical Disease
Lyme disease is an extremely challenging infectious/toxic disease for both doctor and patient. It can exhibit many different symptoms. The clinical picture of LD can be similar to fibromyalgia, including: chronic fatigue, joint pain (arthralgias), muscle, fibrous tissue and tendon pain. Lyme disease can also manifest primarily as a neurological disorder, including fatigue and many neurological symptoms. It is important to remember that there are hundreds of symptoms that are caused by LD and it can mimic many diseases; for this reason, LD is often called, "the great imitator."
The prognosis of Lyme disease depends a lot on how soon the disease is caught and how well it is treated. Early, aggressive, and comprehensive treatment improves the prognosis tremendously. Unfortunately it is difficult to diagnose many cases early because they don’t present themselves with obvious Lyme disease symptoms. They often show only one or a few subtle symptoms that can easily be misdiagnosed as something else.
Lingering Lyme: The Chronic Persistent Infection
Some symptoms and signs of Lyme disease may not appear until weeks, months, or years after a tick bite. This stage typically involves intermittent episodes of joint pain or numerous neurological symptoms such as: meningitis, Bell's palsy, dysfunction of cardiac rhythm, and migratory pain to joints, tendons, muscle and bone. Arthritis is most likely to appear as brief bouts of pain and swelling, usually in one or more large joints, especially the knees. In some patients, the first and only sign of Lyme disease is arthritis. In others, nervous system problems are the only evidence of Lyme disease. However, any combination of symptoms can be present.
Primarily unique to humans, neuroborreliosis (the neurological form of Lyme disease) can include numbness, pain, Bell's palsy (paralysis of the facial muscles, usually on one side and more often the left), and meningitis (fever, stiff neck, and severe headache). Dysautonomia (a dysfunctioning autonomic nervous system) and irregularities of the heart rhythm may occur.
In a minority of individuals (11%), development of chronic Lyme arthritis may lead to erosion of cartilage and/or bone. Other clinical manifestations associated with chronic neuroborreliosis include neurologic complications such as disturbances in memory, mood, or sleep patterns, and sensations of numbness and tingling in the hands or feet (parethesia).
The course of the disease can best be described as persistent, with periods of worsening symptoms, often cyclical every few weeks or monthly. Especially disconcerting are persistent symptoms such as pain, headaches and fatigue. Some patients are more symptomatic than are others, which may reflect gender and genetically-determined differences in response to infection. The disease is progressive, destructive, and debilitating, and in severe untreated cases, it can be fatal.
Chronic Borrelia can also cause a degenerative skin disorder now known as acrodermatitis chronica atrophicans (ACA).
Lyme disease causes metabolic/endocrine dysfunctions that lead to weight loss or commonly chronic weight gain.
Generally, women struggle with chronic Lyme disease more severely than men do. It is not known for sure why.
List of Lyme Disease Symptoms
As I mentioned before, every organ and organ system can be affected, here’s a list of some of the LD symptoms as they relate to specific areas of the body:
One or more of these symptoms is not diagnostic for LD, except for a bulls-eye EM rash. A diagnosis for LD is a clinical one and must be made by a physician experienced in recognizing LD symptoms and history, experienced in interpreting lab results and recognizing a response to treatment. Always remember that negative serological tests are not reliable and cannot be used solely for a diagnosis. These tests frequently are incorrectly negative.
The Diagnosis of Lyme Disease
Lyme disease is diagnosed clinically based on history, clinical symptoms, and response to therapy. No test can conclusively "rule-out" Lyme disease. It is critical to understand that the diagnosis of Lyme disease is heavily weighed on clinical symptoms and history alone. LLMDs are familiar with the complex nature of Lyme disease and are very aware of the subtle symptoms it can produce. Their clinical judgment must be very keen for them to recognize early, subtle cases.
Clinically, "chronic fatigue syndrome" or "fibromyalgia", which is more recently called "chronic fatigue immune dysfunction syndrome" (CFIDS) cannot be readily distinguished from chronic Lyme disease and in fact is probably one in the same disease. Yes, I believe along with many LLMDs that most cases of fibromyaliga and CFIDS are actually misdiagnosed cases of chronic Lyme disease. Strong support for this comes from the fact that antibiotic and other LD therapies improve many patients diagnosed with fibromyalgia.
Routine laboratory tests are usually normal in LD. Liver enzymes may be elevated from hepatitis. The erythrocyte sediment rate (ESR) is most often normal, distinguishing it from some of the purely inflammatory disorders such as rheumatoid arthritis or lupus. However, overlap between LD and autoimmune diseases frequently occur. I believe that the chronic inflammation and immune dysfunction caused by LD often leads to autoimmune diseases. Culture of the Borrelia is rarely possible but can occur in a few early LD cases of B. burgdorferi, usually from biopsies of the EM rash. However, most laboratories are not capable of the difficult culturing of these slow growing borrelia organisms and we have not been able to isolate many borrelia species in the laboratory.
Currently available serological (blood) tests for LD caused by B. burgdorferi include the immunologically-based ELISA and Western blot assays. The problem with the ELISA is the high amount of background compared to Western blot assays, likely due to the use of whole organisms. After correction for the high background, only a small percentage of positives can be detected. Because the Western blots separate the proteins of the borrelia, specific reactions can be seen, and more accurate interpretations of the results made. Clinically over 75% of patients with Lyme disease are negative by ELISA, but positive by Western blot. However, it is important to remember that there are many patients (approximately 30%) who have symptoms, but whose Western blots are negative. The different antigenic profile between Borrelia species along with their ability to avoid the immune system and remain intracellular could explain the absence of immune responses. Even more likely is that the pathology of borreliosis can lead to immune dysfunction. Cells of the immune system can be triggered into apoptosis (preprogrammed death or suicide). The death of cells of the immune system can also explain the dysfunctional immune system and the problems there are using serological laboratory tests to diagnose chronic borreliosis as shown below:
Epidemiol Mikrobiol Imunol. 2001 Feb;50(1):10-6.
Persistence of Borrelia burgdorferi sensu lato in patients with Lyme borreliosis
Honegr K, Hulinska D, Dostal V, Gebousky P, Hankova E, Horacek J, Vyslouzil L, Havlasova J.
Infekcni klinika, Fakultni nemocnice, Hradec Kralove.
In 18 patients with Lyme borreliosis the authors proved the persistence
of Borrelia burgdorferi sensu lato by detection of the causal agent by
immune electron microscopy or of its DNA by PCR in plasma or
cerebrospinal fluid after an interval of 4-68 months. Clinical
manifestations common in Lyme borreliosis were present in only half the
patients, in the remainder non-specific symptoms were found. In nine
subjects with confirmed Borrelia burgdorferi sensu lato in the
cerebrospinal fluid the cytological and biochemical finding was normal. Examination
of antibodies by the ELISA method was negative in 7 of 18 patients
during the first examination and in 12 of 18 during the second
examination. In all negative examinations the specific
antibodies were assessed by the Western blot or ELISA method after
liberation from the immunocomplexes. In the authors' opinion it is
advisable to examine repeatedly plasma and other biological material
from potentially affected organs by PCR and subjects with persisting or
relapsing complaints after the acute form of Lyme borreliosis as well as
to examine cerebrospinal fluid in case on non-specific symptoms and
concurrent pathic EEG or MR findings.
There is a critical need for the development of a better diagnostic test to detect Lyme disease caused by Borrelia species. Until then, the Western blot assay is the best clinical test currently available.
PCR (Polymerase Chain Reaction) is a highly sensitive way to detect microbial DNA and is beginning to play an important role in the diagnosis and research of borreliosis. This technology has the potential to bridge the gap between the clinical diagnosis and the laboratory confirmation.
The Treatment of Lyme Disease
Our understanding of treating this disease has made a great leap recently with the discovery of Dr. Marshall’s work.
The best approach to therapy is a multifaceted and comprehensive treatment regimen that includes conventional antibiotics, numerous complimentary and alternative therapies, and a nutritional regimen specifically designed to reduce inflammation, aid the liver in detoxifying the BLPs, decrease the risk of yeast infections, repair damage caused by the disease and strengthen the immune system.
The mainstay of treating chronic borreliosis is to follow Dr. Marshall’s protocol for sarcoidosis found here: www.sarcinfo.com. This comprehensive therapeutic approach is much more effective than the conventional treatment that uses only a single therapeutic entity such as antibiotics alone.
Antimicrobial Therapy: The Conventional Treatment -- Antibiotics are the foundation of conventional Lyme disease therapy. We are often told by the medical establishment and the general media that Lyme disease is easily treated with antibiotics. Unfortunately, in most cases, this is not true. If caught early, then yes, Lyme disease can be treated relatively well with only antibiotics. But, as I mentioned earlier, most of the time it’s not caught early and once the borrelia has spread throughout the body and secondary symptoms have occurred, treatment gets much more complicated and less effective.
Oral therapy with doxycycline, minocycline, tetracycline or amoxicillin is appropriate for early cases of Lyme disease. Parenteral therapy, usually intravenous (IV) administration, maybe used for patients with neurologic involvement, severe arthritis, or any life-threatening manifestation of Lyme disease such as complete heart block. However, there’s good evidence to suggest that oral therapy can be just as effective if not more so in most cases.
If you can’t find a LLMD in your area and can’t get in to see one on a timely basis there are places you can order prescription medication without a prescription such as this: http://www.edrugnet.com or www.rxsolutions.com.
The treatment of patients with chronic Lyme disease is very controversial. The more I study the chronic symptoms of Lyme disease, the more I believe that the persistence of the disease is caused by a persistent borrelia infection and the persistent or residual presence of fat-soluble BLPs that can depot in the lipid tissues throughout the body and in many cases lead to immune dysfunction. Permanent damage can also occur throughout different stages of disease and cause chronic symptoms to persist.
Borrelia species are sensitive to several oral antibiotics including: amoxicillin, tetracycline, doxycycline, minocycline, clarithromycin (Biaxin®), metronidazole (Flagyl®), co-trimoxazole sulfamethoxazole/trimethoprim (Bactrim® or Septra®) and azithromycin (Zithromycin®).
Early in Lyme disease at the time of the early skin EM rash, any one of the above antibiotics appears to be effective if given for at least 2 months. Antibiotic treatment of only 2-3 weeks is insufficient and patients often deteriorate with chronic symptoms of borreliosis including; arthralgias, fatigue, and paresthesias. Thus, LLMDs recommend that tetracycline, doxycycline, minocycline or amoxicillin be used for at least 2 months if an EM rash is the first and only symptom of Lyme disease.
If any other symptoms appear after an EM rash, the treatment of LD for only 2-4 weeks frequently fails and relapses occur. LLMDs suggest that several months of doxycycline, minocycline or other appropriate antibiotics have a higher success. In patients with symptoms present for more than six months, the treatment course may need to be more prolonged, or a retreatment course of varying length may be needed. In patients with symptoms for more than a year, several months or years may be needed for complete resolution of symptoms. In general, treatment for chronic LD usually requires a period of time equal to or greater than the time the patient has had the disease. The slow growth rate and the cryptic and stealthy nature of borrelia justify the need for longer antimicrobial treatment periods.
When Some Symptoms are a Diagnostic Sign: The Jarisch-Herxheimer Reaction to Treatment
Once treatment is initiated for patients beyond the EM stage, their symptoms frequently increase during the first several days, or even for the first two weeks of therapy. This reaction is called a Jarisch-Herxheimer reaction (herx) and is the body’s response to the BLPs being released from the dying borrelia. These BLPs stimulate the inflammatory cascade which explains this phenomenon. The herx reaction is a very helpful clinical symptom Lyme clinicians use to support a clinical diagnosis of Lyme disease.
For patients with preexisting symptoms of more than a few months, relief of any of their symptoms may not occur until after 4-6 weeks of therapy. Typically, there are short periods of relief, followed by relapsing or migrating symptoms. With continued therapy, there are longer symptom-free periods. Some arthralgias may require several months of therapy to resolve, and fatigue and dizziness may be the last symptom to resolve.
The preference for a variety of antibioitics by some LLMDs is based on a large number of failures that were noted in patients who had been on only amoxicillin, or doxycycline. It seemed that patients generally have some initial relief, but then plateau. It’s not clear if tetracycline is as effective as doxycycline; some claim it is not while others say it is better. There are some physicians who use doxycycline at high doses of 600mg daily to achieve a more successful result. It’s my opinion that low to moderate doses of antibiotics is more appropriate. See the work of Dr. Brown: www.roadback.org.
Metronidazole (Flagyl) is a very effective antimicrobial for treating chronic Lyme disease. It distributes well throughout the body and is able to penetrate tissue and cells. This ability allows metronidazole to reach the cryptic borrelia throughout the body and kill it. Metronidazole is also effective at attacking the cyst form of borrelia. This may be the single most effective antimicrobial pharmaceutical for treating Lyme disease. The disadvantage of metronidazole is it’s toxicity to the liver and neurological system. It can raise liver enzymes and cause peripheral neuropathies similar to LD itself. These side-effects must be prudently monitored.
Of the beta lactams used for the treatment of Lyme disease, the most effective appears to be ceftriaxone (Rocephin). In limited comparitive trials, cefotaxime appears to be equally effective, and high-dose IV penicillin is too. In early stages of LD, oral amoxicillin is as effective as doxycycline. In later stages, however, many failures are noted, despite the use of up to 3 grams of amoxicillin daily.
The newer macrolides such as azithromycin, roxithromyin and clarithromycin are effective. LLMDs often use clarithromycin and azithromycin in higher dosages for longer periods of time than regularly recommended for these antibiotics.
In evaluating all of the possible factors, it would appear that antibiotics that can inhibit the bacteria’s ability to synthesize toxic bacterial lipoproteins and achieve intracellular concentrations are the most efficacious drugs. The results fit with clinical experience that the tetracyclines, (minocycline, doxycycline), sulfamethoxazole/trimethprim, lincosamides (clindamycin) and the macrolides (clarithromycin and azithromycin) achieve the greatest success.
Fortunately, there have been no reports showing any change in antibiotic resistance patterns regarding antibiotic susceptibility of the specific borrelial organisms in a given case.
Again, my personal preference is use of low-dose antibiotics such as doxycycline or minocycline.
Combinations of Antibiotics
Antibiotics used in combination are much more effective than used separately. Several antibiotics work together synergistically to improve the therapeutic effect against borreliosis. Examples of antibiotics that work well together when combined include: amoxicillin, metronidazole, clarithromycin or zithromycin, and co-trimoxazole. Co-trimoxazole works well in late stage Lyme disease, especially when given in combination with other antibiotics like amoxcilliln and/or a macrolide such as azithromycin. Earlier, one exception to antibiotic combinations was the use of metronidazole and the tetracyclines together. It is now believed that these two antibiotics do work well when combined. For example, there are reports of good result when doxycycline is used with flagyl.
Antibiotics that inhibit protein synthesis
Antibiotics that inhibit protein synthesis will also inhibit the production of BLPs by borrelia. This can be a useful tool for reducing the load of BLPs the body must deal with. Since the BLPs trigger the disease and the symptoms of borreliosis, reducing their production would be of significant benefit.
Tetracyclines
The tetracyclines including: tetracycline, doxycycline, minocycline; inhibit protein synthesis in bacteria. They do this by binding to the 30S unit of the bacterial ribosome. This binding blocks the bacteria’s ability to synthesize proteins. Unfortunately, this binding is reversible. So, they must continued to be used until the bacteria die or are cleared from the body.
Macrolides and Lincosamides
The most widely used macrolides for LD are azithromycin and clarithromycin. These are relatively non-toxic antibiotics. Macrolides binds to the 50S ribosomal subunit and inhibits either peptidyl transferase activity or translocation of the growing peptide.
Clindamycin which is a lincosamide, has a similar mode of action as the macrolides.
Adjunct Anti-Microbial Therapies
Hyperthermia – Borrelia prefer temperatures below that of the body. Using hot showers, baths, or saunas at temperatures of up to 104 degrees F for 20-30 minutes daily to raise the body temperature is a helpful therapy for treating borreliosis. Borrelia species are especially sensitive to the combination of antibiotics and heat. Raising the body temperature also dilates the peripheral circulation and increases the permeability of the blood vessels throughout the body. These physiological changes assist in the delivery of antibiotics to all areas of the body increasing the amount of antibiotics able to penetrate and reach the borrelia. Hyperthermia improves the effect of antibiotic therapy by approximately 16 times.
Pulsing Electro-Magnetic Fields (pemfs) -- Recently, there has been a lot of progress in studying pemfs as a therapeutic modality for LD. This information is too numerous for me to list here so I’ll refer to this message board that I follow and participate in where the members discuss pemfs design and therapies.
http://health.groups.yahoo.com/group/Magpulser/?yguid=159339971
Pemfs are very effective in pain and other symptom relief. I highly recommend it’s use.
Here’s a site that lists some of pemfs useful benefits:
http://www.magnetcure.com/reports.html
Rife Machine -- Rife machines are electronic devices that produce varying frequencies of energy (similar to a microwave, but at frequencies not harmful to the body). This energy penetrate the tissues of the body and cause the spiral-shaped Borrelia to resonate so much that the integrity of the bacteria is disrupted; weakening and even killing them. This is an effective means for killing borrelia and is supported by the production of herx reactions in Lyme patients after Rife treatments, while non-infected individuals don’t experience the herx reactions when exposed to rife treatment. Rife machines are not approved by the FDA and are relatively expensive. A reasonable price for a good machine is about $1,000. Homemade ones can be much less expensive and just as effective. Here is a message board that I follow and participate in where the members discuss numerous alternative therapies including rifing: http://health.groups.yahoo.com/group/Lyme-and-rife/
Beck Electrification -- Low-voltage electrification is also useful for disrupting the integrity of microbes including borrelia. It may also enhance the ability of antibiotics to penetrate the cells of the body so they can reach the hidden intracellular borrelia. Herx reactions after treatment also substantiate the effect of this therapy.
Lauricidin -- The monoglyceride of lauric acid is called monolaurin. The concentrated form of monolaurin has potent antibacterial properties. While nontoxic and approved as a direct food additive by the FDA, monolaurin adversely affects bacteria, yeast, fungi, and enveloped viruses. It damages the cell membrane of pathogenic bacteria.
Colloidal Silver -- Colloidal silver therapy for Lyme disease appears to be significantly effective with many individuals that have used it. There is much controversy regarding this therapy. Argyria, is the name of the condition in which the skin turns bluish-gray from silver. This is very rare and is linked to the use of silver salts and not pure colloidal silver. It appears to be important to use pure colloidal silver. The size of the colloidal particles is also important. The smaller the particles size of CS the better the bioavailability, the stronger the anti-microbial effect and the safer to use.
Cat’s Claw / Samento / Saventero – A Peruvian herb (Uncaria tomentosa) is quickly becoming a rising star within the LD community. It appears to have both anti-microbial and anti-inflammatory properties both of which are significantly effective. Tolerance is a question for some. It can cause anxiety, insomnia, and irritability in certain individuals. Adjusting the dose appropriately can control this side-effect. Even at very low doses it seems to be beneficial.
Artemisinin – Is the active constituent of the herb (Artemesia annua). Tea made from this herb has been used in Asia to successfully treat malaria. Artemisinin (pronounced art-ee-MISS-in-in) is the preferred antimalarial therapy. It is also being used to treat cancer in veterinary medicine and is an effective anti-parasite and anti-microbial treatment.
Artemisinin also seems effective in treating LD. There are many testimonials from users claiming significant benefits.
Goldenseal root – The best brand out there is may be Eclectic Institute's freeze-dried goldenseal root.
Teasel – Another effective herbal therapy.
Olive Leaf Extract – (Oleuropein) Must be taken at high doses though. Take 1500 – 2000 mg three times per day.
Garlic – Antimicrobial and helps reduce blood clotting. Use fresh garlic or freeze-dried supplements.
European (or Hungarian) Mistletoe – There is a little information that this may be beneficial for LD as an antimicrobial.
Peroxide – Is a potent antiseptic but I’m concerned about the safety of oral and IV administration.
Ozone – Similar concern as with peroxide.
Controlling Inflammation and the Immune Dysfunction
Inflammation is a major part of any disease, but none more complex and involved than with Lyme disease. Borrelia BLPs that has disseminated throughout the body will trigger inflammation in any and all systems, organs and tissues that it resides in. This is how Lyme can cause so many different symptoms and mimic so many disorders. Dealing with this complex inflammation is a major part of managing Lyme disease. Controlling inflammation begins with a well balanced low-carb diet. Why? Basically because sugars and starch promote inflammation by altering the body’s metabolism of fatty acids. I explain this in depth in my writings on insulin resistance and the inflammatory syndrome (IRIS). The low-sugar/starch diet also reduces the chance for yeast infections to become established. Nystatin (an antimicrobial for yeast) can be taken orally to also prevent yeast growth. (If you would like any more information on the low-carb diet, please refer to my book, "Dr. Taylor’s Remedi for Healthy Living." You can order it on my website at www.myremedi.com. or toll free at 877-736-7348.)
There are several dietary supplements that help reduce inflammation: MSM, Salmon oil, Aflamend™, and LyprinolÒ work well. MSM, Methylsulfonylmenthane (MSM) is a very safe supplement that is used to reduce inflammation without the risk of any side effects. It is inexpensive, but therapeutic doses for an adult are high. Salmon oil is abundantly rich in the Omega-3 fatty acids. The fatty acids EPA and DHA that are found in Salmon oil help reduce inflammation and have many other health benefits. Aflamend™ is a blend of herbal extracts I designed to help reduce inflammation. Aflamend™ augments the health benefits of Dr. Taylor’s "Remedi for Healthy Living" program by improving insulin sensitivity and enhancing a healthy fatty acid metabolism, both of which reduce chronic inflammation.
Lyprinol,Ò a specific stabilized extract of green lipped mussels, is a relatively new supplement for inflammation. Early feedback of LyprinolÒ use is reporting several beneficial results for people with many stubborn inflammatory disorders. This product is a unique fatty acid that is an effective tumor necrosis factor (TNF), lipoxygenase and (LOX) inhibitor. Its potency to reduce inflammation is approximately 200 times stronger than fish oil. It is also an effective MMP-9 inhibitor thus it helps reduce the MMPs that digest the extracellular matrix proteins of the body.
Other inhibitors of TNF include Boswellia, Quercetin, Cat’s Claw, Turmeric, NAC (N-acetyl-cysteine).
Nettle also has the ability to inhibit the release of MMP triggered by BLPs.
Cherry Fruit extract, Cetyl Myristoleate, help inflammation problems.
Other dietary supplements helpful for Lyme patients include: bovine colostrums, lycopene and DHEA to improve growth hormone and other hormone deficiencies, the minerals magnesium and potassium, vitamin C, vitamin E (mixed tocopherols), and a good multi-vitamin that contains no retinyl palmitate form of vitamin A. Vitamin B12 helps deal with neuropathies. It can be taken sublingual (under the tongue) daily or preferably by subcutaneous weekly injections. Other supplements that will help to reduce inflammation and support the immune system include Borage and/or Evening Primrose oil, and DMAE. DMAE (dimethylaminoethanol) helps with fatigue caused by Lyme disease. Astragalus is a herb that is used for immune support.
Protecting the Nervous System from Neurotoxins
It is important to protect the peripheral and central nervous system from the toxins produced by borrelia. The following is a list of dietary supplements that are effective for this:
SAMe: S-adenosyl-L-methionine: The beneficial effects of SAMe supplementation are extensive because this nutrient is involved in so many metabolic processes, including its role in serving to detoxify cell membranes and synthesize neurotransmitters. From acting as an antioxidant to raising serotonin levels in the brain, SAMe is one of the most important compounds to come to the market. Studies on the use of SAMe in maintaining normal joint function are also promising.
Phosphadityl choline: Take 1 tablespoon of lecithin with each meal.
DMAE (dimethylaminoethanol) is a precursor to acetyl choline and has many benefits for LD therapy.
B-vitamins: LD patients need high doses of B-vitamins, especially B-6, B-12, and folic acid.
Anti-oxidant that are effective at protecting the nervous system include: pycnogenol, grape seed extract, bilberry, and alpha lipoic acid.
Detoxifying and Excreting the Toxins of Borrelia
Borrelia produce numerous toxic BLPs. These toxins are important because they trigger many harmful responses in the body including the inflammation that is damaging to healthy tissue, and cause the dysfunction of the immune system. These toxins are fat-soluble lipoproteins and are very difficult to rid the body of. The body normally detoxifies fat-soluble substances in the liver and excretes them from the bile. Unfortunately, the toxins appear to be reabsorbed from the gut and circulate back into the body.
Treatments designed to aid the body in eliminating these toxins is a very important part of a complete and comprehensive Lyme disease therapy.
Glutathione is the most important detoxifying agent in the body to get rid of undesirable toxins such as BLPs produced by borrelia. It forms a soluble compound with the toxin that can then be excreted through the urine or the gut. The liver and kidneys contain high levels of glutathione as they have the greatest exposure to toxins. The lungs are also rich in glutathione partly for the same reason. Glutathione is a small molecule found in almost every cell. It cannot enter most cells directly. Instead glutathione must be synthesized inside the cell from its three constituent amino acids: glycine, glutamate and cysteine. The rate at which glutathione can be made depends on the availability of cysteine, which is relatively scarce in foodstuffs. Furthermore, the cysteine molecule has a sulfur-containing portion which gives the whole glutathione molecule its ‘biochemical activity’, i.e. its ability to carry out its vitally important functions. Glutathione is the major antioxidant produced by the cell, protecting it from ‘free radicals’ (‘oxygen radicals’, ‘oxyradicals’). These highly reactive substances, if left unchecked, will damage or destroy key cell components (e.g. membranes, DNA) in microseconds. Oxyradicals are generated in the many thousand mitochondria located inside each cell, where nutrients like glucose are burnt using oxygen to make energy. (Mitochondria can be thought of as the batteries that provide the power for the cells to operate). High levels of oxyradicals are also generated from inflammation or immune dysfunctions such as in chronic LD.
Thus, glutathione is required in many of the intricate steps needed to carry out an immune response. For example, it is needed for the lymphocytes to multiply in order to develop a strong immune response, and for ‘killer’ lymphocytes to be able to kill undesirable cells such as cancer cells or virally infected cells. The importance of glutathione cannot be overstated. It has multiple roles as indicated and, indeed, as one examines each system or organ more closely, the necessity for glutathione becomes increasingly evident. Glutathione values decline with chronic disease and age. Higher values in older people are seen to correlate with better health, underscoring the importance of this remarkable substance for maintaining a healthy, well-functioning body.
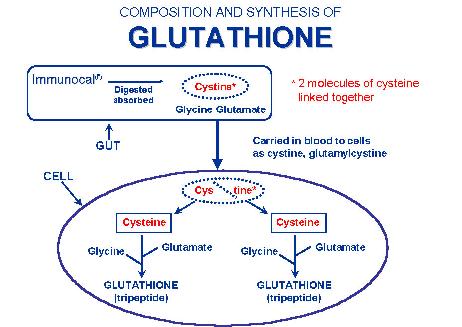
The two dietary supplements, undenatured whey proteins and NAC (N-acetyl-cysteine), are the best cost effective way to increases the production of intracellular glutathione.
The biliary system gives us a chance to trap the toxins while they are in the gut. Substances that trap fat-soluble compounds can be taken orally to do this. Care must be taken not to use these chronically because they can have side effects and reduce the absorption of healthy fat soluble vitamins and nutrients.
Chlorella
Very effective detoxifier
Stimulates the immune system
Contains growth factors that stimulate the regeneration of damaged tissues.
Chitosan: a shellfish fiber that traps lipids.
Bentonite: is a clay-like substance that attracts lipophilic compounds
Apple Pectin:
Cholestyramine (Questran or Cholistad): a prescription that traps lipophilic compounds. Cholestyramine can cause constipation as a side effect.
Milk Thistle: Is probably the best herb that helps the liver detoxify and excrete bile.
Exercise & Sauna: increases the production of bile and mobilizes lipids. Heat therapy is a very effective detoxifying therapy.
Scrubing skin with sponges or brushes enhances the skins ability to remove toxins.
Using fiber (psyllium) to scrub the GI tract removes dead epithelial cells that contain toxins.
NAC (N-acetyl-cysteine): The best supplement that increases the production of glutathione, which is used in detoxification.
Taurine: An amino acid that aids in detoxification by providing a good source of sulfur.
Immune Modulation
Therapies to improve or repair the dysfunction in the immune system are important remedies when dealing with chronic disorders such as LD. The hope of this type of therapy is to tilt the balance of the immune system in favor of defending the body from chronic borrelia infection.
Tick Protection and Prevention
Repellant sprays are a useful tool to reduce exposure to ticks. Products that contain DEET are good tick repellents. They do not kill the tick and are not 100% effective in discouraging a tick from feeding on you. Products like Permanone contain premethrin, and are known to kill ticks. However, they are not designed to be sprayed on the skin. Premethrin can be sprayed on clothing. Once it is dry it is assumed to be safe to touch. Pest resistant clothing can offer some protection. Ticks are anti-gravitational, i.e., they generally seek the highest point on the body. If they get on the body below the clothes line, they will travel up and die once they come in contact with premethrin treated clothing. Note: If the tick meets resistance on its journey to the head, it will stop and feed at that point.
Tick Removal
If an attached tick is found on your body, remove it carefully with fine tweezers. Grab the tick as closely to the skin as possible. Do not squeeze the body; do not apply Vaseline; do not touch the tick with a burnt match; and do not clean it with alcohol while the tick is attached. Any of these actions could cause transmission of Lyme disease by causing the tick to regurgitate the borrelia bacteria that live in their gut into the skin where it is attached. Ticks can be identified and tested for the bacteria. However, Borrelia frequently cannot be grown in the laboratory due to its fastidious nature and so nothing shows up. It’s still important to save the tick for identification as a possible vector. Place the tick in a glass or plastic vial with a few blades of moist grass or a moistened cotton ball. A clean pill vile is good. If none is available, use a Ziploc storage bag as a temporary container.
Stop It Before It Starts
I strongly recommend prophylactic treatment when a person is bitten by a tick, especially if the tick has been attached over 24 hours. Since there isn't enough evidence on either side to prove or disprove this theory, the final decision is up to the individual and the treating physician. The recommended prophylactic treatment is 4-6 weeks of an oral antibiotic. 100 mg doxycycline tid (three times per day) or 1000 mg amoxicillin tid for prevention for at least 6 weeks is recommended.
Vaccine
As of March, 2002, the LymerixÒ vaccine is no longer available. In December 1999, a class action suit was filed against SmithKline Beecham, the manufacturers of the LYMErixÒ vaccine. The complaint alleges the manufacturer failed to warn doctors and the general public that nearly 30% of the general population was genetically pre-disposed to a degenerative autoimmune syndrome, including chronic arthritis, which the lawsuit says, is triggered by the OSP-A contents of the vaccine. We know that the OSP-A contains many of the toxic BLPs that trigger LD. Many private lawsuits have also been filed from individuals who received the vaccine and are now disabled with chronic arthritis. So, this means that a safe vaccine is not yet available to the public.
Animals
Lyme disease can affect individual pets differently. Some animals may display no symptoms. Other animals may develop fever, loss of appetite, painful joints, lethargy, and vomiting. If left untreated, the spirochete may damage the eyes, heart, kidneys, and nervous system. Lyme disease has been diagnosed in dogs, cats, horses, goats, and cattle. Other species may also be at risk.
Infected dogs may be lethargic, have a poor appetite, or a fever. Dogs may also experience lameness shifting from one joint to another, fatigue, kidney damage or failure, heart disorders, or neurologic involvement (e.g. aggression, confusion, overeating, and seizures). Dogs can also be infected with the Lyme bacterium but not exhibit any noticeable symptoms. Transplacental transmission has occurred in dogs.
Many cattle do not display signs of Lyme disease; those that do may have lameness, painful or swollen joints, fever, or weight loss. A skin rash may be present on the udder of infected cows. "Bb" has been found to exist in urine and colostrum of infected cattle; therefore, the possibility of transmission between cows should be considered. The Lyme bacterium has also been found in blood, milk, synovial fluid and spontaneously aborted fetal tissue. "Bb" can survive in frozen milk, but is killed during pasteurization due to its sensitivity to heat.
Infected horses generally do not have a fever, but may have lame or stiff joints, laminitis, depression, or refusal to eat. This bacterial infection may be a cause of moon blindness or loss of vision. There have been reports of spontaneous abortion and encephalitis in horses infected with "Bb". Neurologic signs include head tilt, difficulty swallowing, or aimless wandering. Transplacental transmission occurs. Colts born to infected mares have displayed birth defects. Many horses may be infected with the spirochete, but display no symptoms.
Cats may show lameness, fever, loss of appetite, fatigue, eye damage, unusual breathing, or heart involvement. However, many cats do not show noticeable symptoms, despite being infected.
Humans and monkeys are more susceptible to neuroborreliosis than other animals.
What Can You Do?
First of all, prevention is the best cure. If you have to be outside, use insect repellent with deet. Take a hot shower as soon as you can and check, in your hair especially, for any ticks. Since it is believed that a tick needs to be on your skin for at least 24 hours before spreading the disease, this prevention could save you in the long run. Strongly consider prophylactic antibiotics when bitten by a tick.
If you are suffering with a number of different symptoms and you aren’t quite sure what you have, don’t rule out Lyme disease. This disease is called "the great imitator" and you don’t need a rash on your body to have it. If these symptoms have been going on for a while and you think there is a chance, I would strongly recommend contacting a Lyme disease specialist. One specialist that I know is Dr. Charles Crist in Springfield, MO (417) 886-8389. Here’s his website: www.drcharlescrist.com. For more information about doctors that have worked with LD patients in the state of Iowa, you can contact Judy Weeg who is with the Central Iowa Lyme Disesase Association at (515) 388-1401.
There is Hope
You can find great support at thes websites: www.MarshallProtocol.com and www.lymenet.org
Go to the flash discussion group at lymenet. There are many helpful members of this message group. It’s a great site for support and helpful information.
While many in the medical community are "Lyme ignorant," there are still a few knowledgeable doctors that can be found in Iowa and near the borders. Some people that have been diagnosed with Lyme disease have been given the right treatment for a long enough period to fully recover and are cured. Others carry it and battle with it the rest of their lives. There are others, however, who have been misdiagnosed and mistreated who continue to live with the problems of Lyme disease and they never fully recover. In 1999, two Iowans in their 30’s died unexpectedly from the unknown complications of Lyme disease. As the word spreads about the complex nature of this disease, the hope is that more doctors will begin to learn about Lyme, and will take the actions necessary to fight this disease. It is critical that the public and the medical community are made aware of the true prevalence and dangers of borreliosis. Until this gap of ignorance is filled, many unfortunate individuals will suffer needlessly with Lyme disease.